Pododermatitis is a term given to describe inflammatory disease of the skin of the feet. Signs can vary from just erythema (redness) of the pedal skin, to alopecia, swelling, nodules and “cysts”, ulceration, crusting, draining tracts and hyperkeratosis.
There are a multitude of causes, which can make a correct diagnosis and treatment of the condition difficult. This blog will concentrate on some of the more common cases that I have seen, but here is a list the general categories and diseases to be considered as differential diagnoses for pododermatitis.
| Infectious | Malassezia (yeast) Superficial bacterial pyoderma Deep bacterial pyoderma (furunculosis and “interdigital cysts”) Dermatophytosis (Ringworm) Leishmaniasis (in pets that have travelled abroad) Canine Distemper Virus (“Hard Pad”) Feline Calicivirus Cowpox Infection (Cats) |
| Parasitic | Demodex mites, Sarcoptes mites, Hookworm larvae |
| Allergic | Canine Atopic Dermatitis, Food Allergy, Contact Allergy |
| Immune -Mediated or Autoimmune Skin Disease | Pemphigus foliaceus, Pemphigus vulgaris, Bullous pemphigoid, Vasculitis, Lupus , Plasma Cell Pododermatitis (cats) |
| Metabolic | Hepatocutaneous syndrome |
| Genetic | Zinc-Responsive Dermatitis in Sled Dogs, Familial Footpad Hyperkeratosis, Acral Mutilation Syndrome |
| Traumatic | Foreign Bodies (another cause of “interdigital cysts”) |
| Acquired | Idiopathic nasodigital hyperkeratosis, Sterile pyogranulomas (another cause of “interdigital cysts”) |
| Tumours | Histiocytoma, Squamous cell carcinoma of nail bed, Epitheliotrophic Lymphoma, Calcinosis circumscripta |
| Chemical | Irritant Contact Dermatitis |
| Psychogenic | Acral lick dermatitis (Lick Granuloma) |
When presented with a case of pododermatitis, as with all skin cases, I take note of the age, breed and sex of the animal, get a full history from the pet owner and perform a full clinical examination before examining the feet. I will ask questions on how the animal is housed, how much exercise it has, where it is exercised, what it is food is being fed and how long the pododermatitis has been a problem.
Do the owners have any skin problems? (for instance, in cases of scabies). If a chronic problem, is it seasonal or non-seasonal? Has the animal travelled abroad? (Leishmaniasis). During the clinical examination I will look for evidence of abnormal weight bearing on each foot, look for evidence of systemic illness that may occur with hormonal diseases such as hypothyroidism or with liver disease (hepatocutaneous syndrome).
I will check each foot in turn, examining the pads and both upper and lower surfaces of the foot looking for signs of inflammation, thickening of the skin and pain. Clues as to the cause of the problem can often be seen after doing this, for instance in cases of atopy where there may be inflamed skin elsewhere or just the addition of inflamed ears.
Usually, I will perform skin scrapings and hair plucks to check for evidence of demodex mites, Sellotape impressions taken from the skin surface, which are stained and examined microscopically, looking for evidence of yeast infection. If nodules or discharging lumps are found, then more samples for cytological examination are taken.
Once I have the full history, completed a whole-body clinical exam and in-depth examination of the feet and conducted my basic diagnostic tests, I will have come up with a more narrowed-down list of differential diagnoses and will know what to do next to get a diagnosis. What follows are some photos of the variety of pododermatitis cases I have personally seen. It is not complete at showing every cause and I have seen quite a few cases of conditions I have not listed here but did not have my camera to hand!
I will spend a bit more time talking about the frustrating issue of what are incorrectly called “interdigital cysts” which have several causes, ranging from bacterial furunculosis to sterile pyogranuloma to foreign bodies.
Infectious Causes
1.Bacterial
Bacterial infection of the feet is invariably secondary to an underlying cause such as parasites, allergies or systemic disease. Poor conformation and excess weight can also have a major bearing on this developing because if haired skin ends up becoming in contact with the ground, if the toes are splayed apart, trauma to the skin can develop that allows the hair follicles to become infected.
The haired skin can thicken up and become “false pads”. Many cases of pedal nodular furunculosis on the top surface of the foot are caused deep infection of the hair follicles on the underside of the foot. The follicles can rupture, releasing hair shaft material into the dermis, where is elicits a “foreign body” reaction which can present as a swollen nodule or appear as if it were a cyst.

Pedal Furunculosis in a Dog

Interdigital Pyoderma

Pedal Furunculosis and False Pad Formation

Pedal Furunculosis and False Pad After Antibiotics
Treatment of theses cases involves prolonged courses of antibiotics, often lasting many months. Topical therapy with antibacterial shampoos and soaks in an Epsom Salts bath (to draw out the infection) are also of some use. Some of these cases are actually sterile and respond to immunosupressive doses of steroids or to cyclosporin.
Typical breeds for developing interdigital furunculosis are Giant breeds such as St Bernards, and Great Danes or the bull breeds, particularly English Bulldogs and English Bull Terriers, The bull breeds are also prone to developing atopy, which can be a primary cause of causing pedal inflammation.
They also have tough short hairs on the interdigital skin that is easily driven into the deeper layers. Conformation play a huge part in the cause of many of these and sometimes the only way of dealing with these cases, if medical therapy fails, is surgery called a Fusion Podoplasty or more recently, cutting out all affected tissue with a CO2 or diode laser. A large percentage of cases of so -called “Interdigital Cysts” are caused by one or other of these conditions.
One unusual case of a bacterial infection I saw recently was a case in a cocker spaniel with all four feet affected by a surface and superfical pyoderma (not involving the deeper layers of skin), but nonetheless causing a major problem for the poor dog, caused by a very nasty bacteria called Pseudomonas.
This bacterium is present in the environment and loves moist conditions in which to thrive. The combination of a mild allergic dermatitis and a very thick long hair coat that was made wet by licking, had allowed pseudomonas to get established. It produces enzymes that eat away at the skin , causing ulceration, leading to oozing of serous fluid, further feeding the bacteria.
Pseudomonas is a bacteria capable of producing biofilms,which need to be physically broken down to allow antibacterial therapy to be effective. This case was resolved by closed clipping of the feet which removes the hair (a major surface for biofilm to attach to) and daily washing and application of hypochlorous acid gel (Vetericyn Hydrogel)

Pseudomonas Pododermatitis in a Cocker Spaniel
2. Yeast
Many cases of pododermatitis I see are caused, in part, by a yeast called Malassezia. A large proportion of these cases are also suffering with allergy, but the secondary yeast infection can be contributing as much as 90% of the inflammation and pruritus.
This is one reason I always examine tape strip preparations from the feet under the microscope to look for the Malassezia organisms. Often one sees a brown waxy build up on the underside off the foot in theses cases

Malassezia Pododermatitis
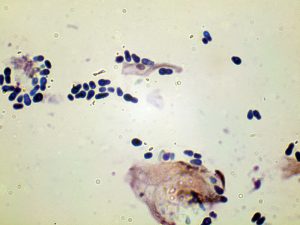
Malassezia Pachydermatits Photomicrograph
3. Viral
In dogs, Distemper virus can cause, along with other symptoms, a condition called “hard pad”. I have no photos of this as I have not seen a case of Distemper for 28 years, thanks to vaccination and herd immunity in the UK dog population, but I saw a very large number of cases in the 1980s when I started out as a vet.
Hard pad is a basically a thickening of the cornified layer (hyperkeratosis) which can also affect the nose. This is a minor problem compared to the much more serious problem of damage to the central nervous system that can occur with this disease!
In cats, I have seen cases of pododermatitis causes by Calicivirus (one of the cat flu viruses) and Cowpox virus. Calicivirus infection is not common, due to vaccinatiom, but if a cat is infected, the disease can cause a fever, nasal discharge and ulcerations in the mouth and on the tongue.
Cutaneous lesions are not as common, but include ulcerations of the footpads, nose, face and pinnae of the ears. Cowpox, despite its name, is caught from rodents. It starts with an initial lesion, often ulcerated, at the point of entry from a rodent bite, usualy the feet or the face, and then 1-3 weeks later, as viraemia develops, small crusted lesions can appear all over the body. It is usually self curing within a few weeks, but is a public health risk to immunocompromised owners.

Feline Calicivirus Pododermatitis

Cowpox Ulcer in Cat Foot
Parasitic Causes
Demodex Mites
Demodex canis and the other two species, Demodex cornei and Demodex injai are probably present in all dogs. In fact, is it probable that every mammalian species has its own species of Demodex that has evolved over millions of years, to live inside the hair follicles as a commensal organism. Humans have two species, Demodex folliculorum which lives in the eyelash follicles and Demodex brevis which lives on the face and nose.

Demodex brevis mite from human face
In dogs at least, the normal population of mites is so small (being kept in check by the immune system) that they are not found on skin scrapings or hair plucks unless they are present in much larger numbers. There are two reasons for over-proliferation of the mites.
The most common is genetic and is seen in young animals and termed juvenile – onset demodicosis and certain breeds are over represented, such as the Bull breeds, Chinese Shar-peis and Boxers. Something is lacking in the young animal’s immune system that allows the mite to proliferate and the mites are thought to produce substances that further suppress the immunity to the mite, allowing huge numbers of demodex mites to develop inside the hair follicles, caused hair loss and allowing secondary bacterial infection to develop.
The second type of demodicosis we see is adult-onset demodicosis and is usually associated with immune supression cause by severe systemic illness or, very commonly, from steroids either if the animal has started producing too much of its own steroids in Cushing’s disease, or if it is on long term steroids for allergy or immune-mediated diseases.
I have seen many cases of atopic dogs that have come to me for second opinions, where the treatment they were receiving (steroids) has “stopped working” when what had actually happened was the long term use of steroids had allowed these mites to proliferate and cause a dermatitis that looks very similar to that caused by atopy (pododermatitis, hair loss, hyperpigmentation and lichenification (thickening) of the skin etc.
A full article in this mite is beyond the scope of this blog but the presence of this mite is the main reason why every case of pododermatitis needs either hair pluck or skin scrapings or both taken for microsopic examination. Until 2-3 years ago, this was still a difficult condition to treat.
Forty years ago dogs were often euthanased as there was only one, not very effective and extremely toxic product called Rotenone, available. Then came a topical treatment caled Amitraz,that was smelly and had to be applied topically all over the body, weekly for months.
We often used off-licence drugs such as Ivermectin orally, again for several months, but treatment is now very easy with the new generation of Isoxazoline insecticides such as Bravecto and Simparica.

Pustular Demodicosis

Demodicosis Dermatitis

Demodex canis mites adjacent to hair root

Demodex canis Mites from Skin Scraping

Demodectic pododermatitis and false pad formation
Allergic Causes
Both Atopy and Food allergy can cause pododermatitis. Usually the feet are just one of the areas affected, as both diseases can also cause inflammation and pruritus on the underside of the body, particularly the axillae, around the perineum, and on the face and ears.
Foot licking is common and in some dogs the only evidence of there being a problem is the brown saliva staining of the hair around the feet that is very noticeable in dogs with light coat colours.

Saliva Staining of Feet in Allergic Dog

Saliva Staining of Foot in an Allergic Dog
Sometimes the inflammation is very subtle and hardly noticed by the owner, but in most cases the inflammation of the underside of the feet particularly, is fairly obvious.

Atopic Dermatitis on Foot

Erythema in Atopic Pododermatitis
A large percentage of these cases are also complicated by secondary Malassezia infection and treatment with topical antifungals, such as Chlorhexidine, can reduce the amount the of foot licking significantly. Treatment of atopic dermatitis is beyond the scope of this blog but further information can be found on this site’s Atopy page .
Immune-Mediated or Autoimmune Causes
There are a variety of autoimmune skin diseases where the immune system attacks either the basement membrane of the epidermis (eg Bullous pemphigoid) or adhesion molecules between individual epidermal cells (eg Pemphigus foliaceus) or blood vessels (vasculitis).
Pododermatis is rarely the only symptom with these diseases, lesions of ulceration and /or crusting developing in other parts of the body. Diagnosis is made in histopathology of skin biopsies taken from lesions/edges of lesions. Treatment usually involves giving drugs such as high dose steroids, Cyclosporin or occasionally a combination of Tetracycline and a B vitamin Niacinamide. Cases of vascultis can be secondary to other diseases and are often treated with Pentoxyfyline.

Ulceration of Footpads in Pemphigus vulgaris

Pemphigus foliaceous Pododermatitis
Metabolic Causes
Hepatocutanteous Syndrome, also know as Metabolic Epidermal Necrosis or Superficial Necrolytic Migratory Erythema is sometimes seen in dogs with chronic liver disease or with glucagon-secreting pancreatic tumours. Pododermatitis is just one of the skin lesions associated with the disease.
Skin lesions consist of bilaterally symmetrical ares of erythema (reddening of the skin) scaling , crusting and erosions on the lower limbs , around the eyes and mouth and genitals. The footpads are hyperkeratotic with splits and ulcerations and lameness is common as a consequence.
Histopathological findings are very similar to that seen with Zinc – responsive dermatoses. Due to the cause , prognosis is very poor unless a resectable glucagonoma can be removed and treatment is aimed at softening that pads to help prevent fissure formation and other topical therapy to help with the scaling and crusting.
Oral Supplementation with amino acids or egg yolks and chicken stock, zinc and essential fatty acids can also help improve the appearance of the skin lesions.

Hepatocutaneous Syndrome Crusting

Pododermatitis Caused by Hepatocutaneous Syndrome
Genetic Causes
Type 1 Zinc-Responsive Dermatosis in Huskies and Malamutes is due to an inherent inability to absorb adequate levels of Zinc from the diet. The distribution of the lesions is very similar to that seen in Hepatocutaneous sydrome. Crusting, scaling, erythema and alopecia occur around the eyes, mouth, genitalia and on the lower limbs and hyperkeratosis of the footpads can develop.
Type 2 Zinc-Responsive Dermatosis is seen in young growing puppies of any breed that are fed high cereal diets, which contain substances called phytates, that hinder absorption of zinc from the intestine. Lesions are very similar to those seen in Type 1 and respond rapidly to change of diet and zinc supplementation.

Type 2 Zinc Responsive Dermatosis

Type 2 Zinc – Responsive Dermatosis
Tumours
Many skin tumours can affect the feet and can cause lameness and due to their presence, can lead to secondary infection with bacteria and yeasts. Tumours such as Melanomas , Mast Cell Tumours, Spindle Cell Tumours, Plasmacytomas, Histiocytomas and Papillomas can all affect the feet. Prognosis is dependent on the diagnosis , which usually made by skin biopsy and histopathological examination

Histiocytoma Adjacent to Claw

Inverted Papilloma on Dog’s Foot
Papilloma could more correctly classes as viral as it is caused by a papilloma virus and is seen in young or immunocompromised animals. Histiocytomas are also more commonly seen in young animals and usually spontaneously regress. They are most commonly seen on limbs or around the head. Occasionally they can be seen on the foot.
Miscellaneous
Calcinosis Circumscripta is a focal area of calcification that develops on areas of repetitive trauma/pressure, such as the footpads or at sites of bite wounds or repetitive choke chain trauma. Surgical excision is usually curative.

Calcinosis Cirumscripta
Steroid-Responsive Footpad Hyperkeratosis in a Cat.
In 2013 I saw a case of severe footpad hyperkeratosis affecting all footpads in 2 year old domestic short hair cat that had developed over a 5 week period. There were no lesions elsewhere on the skin and the cat was otherwise fit an healthy.
Routine bloods were all normal and the cat was FIV/FeLV negative. Biopsies showed severe hyperkeratosis and there was a mild lymphoid reaction around the blood vessels deep in the pad and near the basement membrane of the epidermis. The pads were so hard that a normal punch biopsy could not be used, so we had to take a wedge out of the metacarpal pad using a scalpel.
The case was discussed among several UK histopathologists and an international histopathologist’s discussion group and it would appear that this condition is extremely rare as nobody knew what the cause could be! It did however respond completely to immunosuprressive doses of steroids and remain in remission on a lower dose of steroids.
Stopping treatment resulted in relapse. To this day, I don’t know exactly what the cause was, but it had similar histopathalogic similarities to human psoriasis which is also an autoimmmune disease, so I would probably class this condition as an immune – mediated hyperkeratosis.

Steroid-Responsive Footpad Hyperkeratosis in a Cat

Steroid-Responsive Footpad Hyperkeratosis in a Cat After Treatment
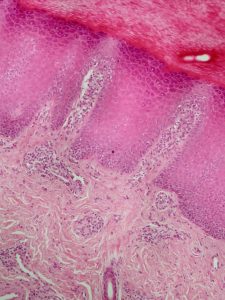
Histopathology Feline Footpad Hyperkeratosis
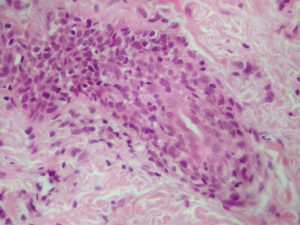
Histopathology High Power Feline Footapd Hyperkeratosis showing lymphocyte reaction around blood vessels
As you can see for the photos in this blog, Pododermatitis can manifest itself in may different ways, but several different conditions can look very similar.
Diagnosis is not always easy and treatment, as always , depends on the cause, but can be prolonged and sometimes be necessary indefinitely.
If your pet is suffering with pododermatitis make sure the cause has been identified and correct treatment given. If necessary, either ask for a second opinion from, or ask to be referred to, a Veterinary Dermatologist.

